This article appears in the Spring 2017 digital issue of DOCUMENT Strategy. Subscribe.
Image by: Digital Vision., ©2017 Getty Images
The Centers for Medicare & Medicaid Services (CMS) is the centralized governing agency that annually publishes all requirements and benefit language, which must be followed by Medicare plan providers. Depending on how the insurer implements model language across its plans, managing these annual updates can be a complex and labor-intensive process.
Most insurers we've talked to cite model document change management as a significant barrier for getting the required communications to market each year—and the stakes are high. The insurer's "Star Rating" can be negatively affected if there are inaccuracies in the information sent. Moreover, missing the required delivery dates for specific communications such as the Annual Notice of Change (ANOC) and Evidence of Coverage (EOC), which are mandated by the CMS, can result in hefty financial penalties. For these reasons, improving the organization's ability to make quick updates, which are 100% accurate, is critical.
Understanding that these challenges will continue to present themselves year-after-year with new CMS requirements, it's not hard to make a compelling case for automating the content management process. Finding a solution for centralizing the content creation and change management process is a good start. Cloud-based, software-as-a-service (SaaS) content management solutions continue to be one option worth considering. They enable a provider to deploy a user management system that provides centralized access to master plan language through an easy-to-use interface while also controlling individual and group rights for changing content through business rules.
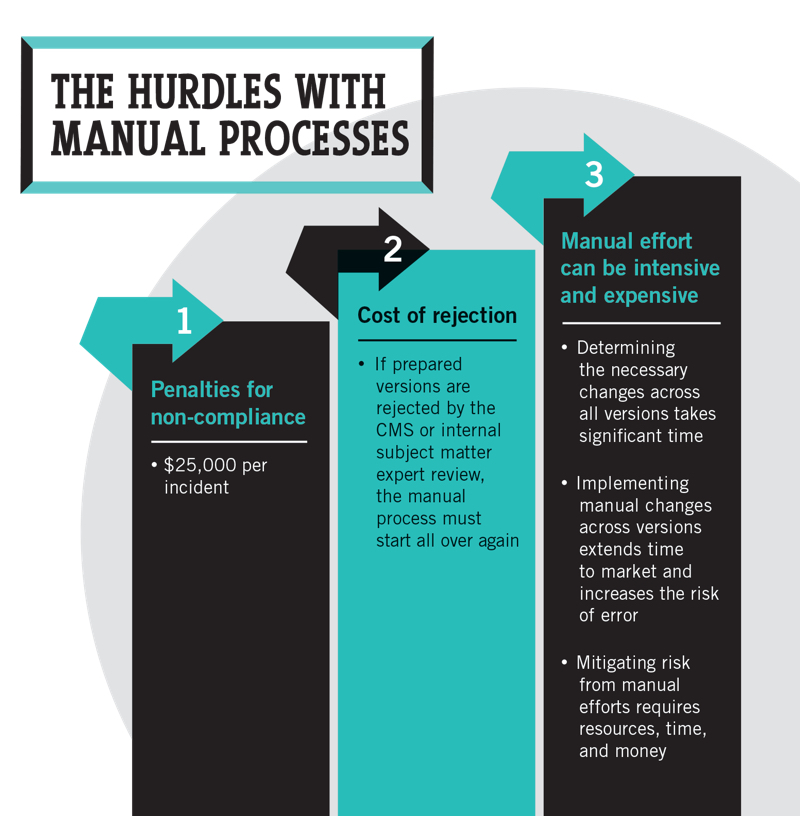
©2017 DOCUMENT Strategy Media
One benefit with an integrated SaaS workflow system is the ability to control all the required steps for creation, edits, and approvals of content changes. Collaboration among internal and external stakeholders is then automated, controlled, and auditable to ensure governance and compliance with required regulations. Additionally, real-time testing and proofing headaches are eliminated through the user interface without the need for information technology (IT) involvement, improving time to market and accuracy of information.
Many providers have found that adopting a centralized content management system enables additional efficiencies through the ability to propagate content updates across all applicable contracts or plan-based material versions. Change approvals can then be made globally or at the version level, which are all controlled by rules to ensure that only approved content is used in production.
A centralized approach of this kind goes a long way toward reducing the risk of managing complex content assembly documents. Greater benefits can also be found by applying the same concepts to letter correspondence, ID cards, monthly and annual health statements, and other member services communications.
Medicare plan providers that employ cloud-based content management technologies are simplifying the process of producing CMS-mandated plan communications, as well as streamlining the production of other documents in the member life cycle. In realizing this level of efficiency, the risk of penalties and operating costs are lowered, and the opportunity to differentiate from the competition and enhance the customer experience is increased.
Nick Romano is Co-Founder and CEO of Messagepoint and is an expert in the customer communications management space. Over the years, Nick has helped many Fortune 1000 companies transform the way they communicate with their customers. Contact him at nickr@prinova.com. Follow Prinova on LinkedIn and Twitter.